BLOG: Key takeaways from the Alliance 2018 Aligning Risk, Quality and Clinical Informatics Value Visit
Kristin Rodriguez, Health Plan Alliance
06/21/2018

Earlier this month, Health Plan Alliance leaders in informatics, quality and risk adjustment explored how health plans are re-engineering how they manage and leverage the data sets critical to clinical decision support and population health efforts. One of our case study presenters, Karen Bray, VP, Clinical Care Services at Sentara Health Plans, said it perfectly, “We’re trying to achieve the quadruple aim—cost, quality, patient satisfaction—but also provider satisfaction.”
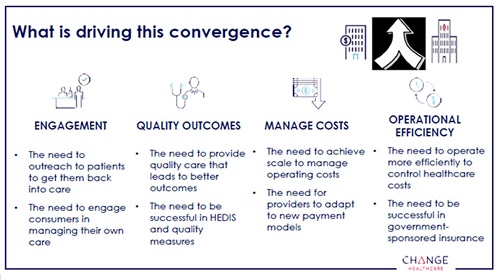 It’s not going to be easy. Alliance members are competing in an environment where health care players are converging, which means they are amassing huge repositories of population health data, plus the resources to put it to use. Change Healthcare’s Jimmy Liu, VP, Risk Analytics Services, highlighted the drivers of this convergence, but also pointed to the environmental factors within which these mergers are occurring. The rise of consumerism, system inefficiency, growing adoption of value-based care, tough regulations and compliance requirements, and data and digital innovation like never before. The great news is, Alliance member health plans tend to outperform national payers in many of these areas—our unique relationships with our provider owners and partners, and our deep understanding of the local communities within which we operate, position us to be nimble and seize competitive advantage.
It’s not going to be easy. Alliance members are competing in an environment where health care players are converging, which means they are amassing huge repositories of population health data, plus the resources to put it to use. Change Healthcare’s Jimmy Liu, VP, Risk Analytics Services, highlighted the drivers of this convergence, but also pointed to the environmental factors within which these mergers are occurring. The rise of consumerism, system inefficiency, growing adoption of value-based care, tough regulations and compliance requirements, and data and digital innovation like never before. The great news is, Alliance member health plans tend to outperform national payers in many of these areas—our unique relationships with our provider owners and partners, and our deep understanding of the local communities within which we operate, position us to be nimble and seize competitive advantage.
RELATED RESOURCE: HealthScape Advisors Value Based Payment Survey Summary: Take away #4 – Transformation capabilities within care management, data management, and analytics are viewed as critical drivers of success under VBPMs.
But even for provider-sponsored plans, helping providers become good at dealing with data, things like sharing documentation with other parties to improve patient care, improving documentation capture and alerts in EMRs, and managing data so that it becomes understandable and actionable, is a tall order. One of the highlights of the value visit was a panel of local primary care providers, collectively representing primary practices of various sizes and with various degrees of EMR adoption and interoperability with their payer partners. The panel was led through a series of discussion topics by MediGold VP, Network Management, Matt Barrett, and one of our panelists finally asked the payer audience in frustration, “Why is it I take so much time to enter data into this EHR, and you still can’t get your hands on it?” Our thoughts exactly.
UPCOMING EVENT: Risk-based cybersecurity, HITRUST, Managing Contract Risk, and National trends in cybersecurity will be covered at our August 7-9 Value Visit. Information Security and ERM experts discuss how to balance the business needs for data sharing with the associated risk.
Top takeaways from the provider panel
Our panel of PCPs didn’t chalk it all up to ongoing disappointment in technology, however. The panel had a great deal of insight to share with the Alliance members in attendance.
One panelist stressed that patients expect their doctor to be a “friend, a confidant and an advisor.” Increasingly, doctors are finding it challenging to manage the growing list of care gap closures they receive from health plans alongside what the patient wants and cares about. One provider reflected on a recent experience when seeing a patient. At the end of the appointment, the patient finally asked, “so… do you have time to hear about why I’m here?” The provider had been using the whole time to “burn through my agenda, rather than starting with the patient’s actual impetus for making the appointment in the first place.” The extra things providers are asked to do during patient visits for Star Ratings often feel like a waste of time because it isn’t helping the patient today. And it’s especially hard because the documentation is buried deep inside the EMR. That being said, they did agree on the preferred incentive for completing additional administrative work associated with a quality bonus: provide incentives for chasing charts and information. These providers use that income to either supplement the administrative staff bonus pool or will pay for a dedicated FTE.
So what would be helpful? Do’s and Don’ts
DO …
- Contact members directly with calls to action, and then just inform the provider.
- Find the right channel for member communications.
UPCOMING EVENT: Provider Partnerships strategy, the secret formula to member engagement, and flexible benefit design are all part of our Government Programs Value Visit this August.
- Put yourself in a patient’s shoes and behave the way the patient wants you to behave. Look hard at things like member incentives, cost sharing, claim approval processes and how you can help with scheduling.
UPCOMING EVENT: Attend our Member Experience Value Visit September 12-14 to learn what other regional health plans are doing to foster both rational trust and deeply felt affection among their members.
- Recognize that physicians struggle to trust business people from the health plan side. Finding strong physician leadership within your organization to build strong working relationships with your provider partners is critical to success.
DON’T …
- Be a tattle-tell. Any communication a health plan sends to a provider regarding member non-compliance (Anything that says, “Did you know that …”) is not received well. Rather than advising providers when patients have care gaps or aren’t filling their prescriptions, reach out to the patient directly to help solve the problem
- Be the payer with a reputation for inaccurate data. These PCPs work with lots of payers, lots of reports, and many of them are not accurate. It boils down to alert fatigue.
- Push 300 pieces of paper or pop ups on December 1st because you’re working on a last-minute, end of year push. There’s no way to get all of those patients in that month.
Gaining insight directly from providers was a powerful addition to the meeting’s discussions, as they are on the front lines when it comes to member compliance and engagement in their own health care, and continuing to align payment models with health outcomes requires a powerful spirit of collaboration. Additional value Alliance member health plans bring to that equation can be found in our ability to power the shift to advanced payment models and population health via strategic data deployment. Sentara Health’s Karen Bray said that when it came to launching their MLTSS program, she realized early on that, “we couldn’t just throw providers at the problem. It’s the headwinds preventing care, not a problem with the care itself.” In other words, when claims and care management data doesn’t tell you the full story about the risk nascent in your population, you must leverage non-clinical data to develop interventions which will meaningfully impact that population’s outcomes, and support your providers’ success.
RELATED RESOURCES
Presentation: Social Determinants of Health LTSS Program Launch
Sentara (Optima Health) shares an LTSS program launch case study accomplished by applying data aggregation and analytics with an eye on social determinants into their clinical data sets.
Presentation: Mission Health Partners case study
Using social determinants data to drive population health operations: Mission Health Partners describes their experience with an automated approach to using social determinants of health data and it impacts our clinical care
UPMC Prescription for Wellness: A Quality Improvement Case Study
This article describes the use of Lean Six Sigma in a quality improvement (QI) effort to design an effective and scalable method for physicians to prescribe health coaching for healthy behaviors in a primary care medical home within a large integrated delivery and financing system.
 Kurt Waltenbaugh built on this notion, and highlighted that only two to three percent of Americans practice four or five of key health habits, including: Not smoking, leading an active lifestyle, maintaining normal body fat, eating a healthy diet, and only drinking moderately or not at all. What’s more alarming for managed care organizations … 11 percent of Americans do NONE of these. The analysis of consumer data provides important, correlative data that adds new, actionable insight—a whole new way of thinking about the hockey stick graphic that illustrates rising health care costs associated with our populations. Members often cross thresholds throughout their time in our care, and often our goal is to prevent them from crossing the next threshold. Without appropriate interventions, members can progress from no chronic conditions, to suddenly having one… and from managing a chronic condition to treating it… from treating it to mitigating related comorbidities, etc. What social determinant data provide is a guide to better navigate the path through which managed care organizations can better engage with the populations who don’t have any claims—both those we believe to be healthy and those we believe to be at risk.
Kurt Waltenbaugh built on this notion, and highlighted that only two to three percent of Americans practice four or five of key health habits, including: Not smoking, leading an active lifestyle, maintaining normal body fat, eating a healthy diet, and only drinking moderately or not at all. What’s more alarming for managed care organizations … 11 percent of Americans do NONE of these. The analysis of consumer data provides important, correlative data that adds new, actionable insight—a whole new way of thinking about the hockey stick graphic that illustrates rising health care costs associated with our populations. Members often cross thresholds throughout their time in our care, and often our goal is to prevent them from crossing the next threshold. Without appropriate interventions, members can progress from no chronic conditions, to suddenly having one… and from managing a chronic condition to treating it… from treating it to mitigating related comorbidities, etc. What social determinant data provide is a guide to better navigate the path through which managed care organizations can better engage with the populations who don’t have any claims—both those we believe to be healthy and those we believe to be at risk.
RELATED RESOURCE
Presentation: Solving Social Determinants of Health before they become claims
Carrot Health presents on solving social determinants of health before they become claims at the Risk and Quality event in Columbus OH, June 2018
With great challenges and great opportunities before us, Alliance members used the balance of the value visit to discuss how we can move the needle and find those important opportunities to realize (and celebrate!) the small wins along the way. Leaders agree that quality, risk adjustment and informatics make powerful teams when working collaboratively. Case studies shared by member health plans offered ways our health plans are thinking about these challenges, and developing solutions.
RELATED RESOURCES:
Presentation: Silo busting between risk adjustment and quality data
Paramount Health's case study describes how their risk adjustment and quality teams are collaborating and aggregating data to improve provider engagement and outcomes.
Presentation: Case Study on Implementing Annual Wellness Visits
Health New England shares a case study on implementing Annual Wellness Visits in conjunction with Baystate Medical Practices, and providing member education and incentive programs.
Presentation: Investing in data sharing with provider partners
Community Health Plan of Washington shares a case study on how investing in data aggregation, management and analytics providing insights to deliver better care.
To post comments, Click Here to Login
